EDITORIAL
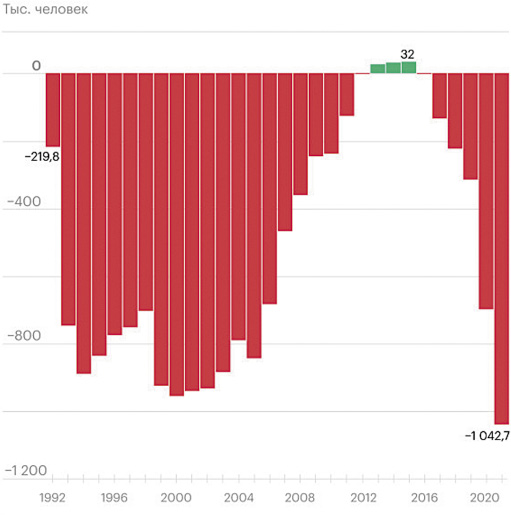
The article examines current demographic trends in Russia in comparison with population changes based on data from the Federal State Statistics Service of Russia (Rosstat) and the UN Population Division. The specifi cs of the age structure of the population of Russia, formed by a number of demographic waves, are such that changes in the number of births and the size of age groups occur in waves; this trend will continue in the coming decades. The state policy of the Russian Federation in the fi eld of family support, aimed at increasing the total fertility rate from 1.3 to 1.6 by 2030 and to 1.8 by 2036, should provide for the introduction of new health-preserving and reproductive health protection technologies, the development of childhood infrastructure, antenatal clinics and perinatal centers for high-quality and aff ordable medical care for mothers and children.
REVIEWS
Background. Birth trauma is a group of diseases caused by mechanical factors during childbirth. Birth trauma is an interdisciplinary problem, affecting various fields of medicine, such as obstetrics, pediatrics, child neurology and other sciences. Birth trauma occupies an important place in the structure of perinatal morbidity and mortality. Birth injuries of newborns during vaginal birth occur in 3.6% of cases, during cesarean section — in 1.2%. However, at present, despite a comprehensive study of the problem, the incidence of birth trauma in newborns remains high. Along with obstetric birth trauma, spontaneous birth trauma also occurs — not associated with any obstetric care.
Purpose of review. To summarize and analyze the available data on the causes of birth trauma in newborns depending on the type of birth injury.
Materials and methods. The review includes published data over the past 10 years regarding the study of the causes of the main types of birth injuries in newborns. The literature search was conducted in Web of Science, Google Scholar, PubMed, and ELibrary databases.
Results. The problem of fetal-pelvic disproportion in the genesis of the development of risk factors for maternal-fetal trauma remains relevant. Fetal macrosomia is one of the most significant factors in birth trauma. The most common skull injury in newborns is cephalohematoma. According to the mechanism of occurrence, birth trauma is divided into spontaneous — occurring during physiological childbirth — and obstetric — associated with any obstetric benefits. The degree of configuration of the fetal head plays a significant role in the pathogenesis of birth trauma. Birth trauma is considered as a systemic reaction on the part of the newborn’s body, which leads to a breakdown of compensatory and adaptive mechanisms and the development of critical damage to the central nervous system and is differentiated from birth damage, which includes only local changes.
Conclusion. To search for preventive measures aimed at preventing birth injuries in newborns, it is necessary to systematize the groups of causes that influence the increased risk of birth injury. Timely assessment of the pathological configuration of the fetal head is extremely important when deciding on the advisability of using obstetric aids during vaginal operative delivery, since it is an early predictor of the formation of fetal-pelvic disproportion — a significant factor in birth trauma in the newborn. In recent years, taking into account the active study of molecular genetic mechanisms in the genesis of the formation of various pathological conditions, the search for various genetic and epigenetic factors that influence the risk of developing birth traumatic injuries in a newborn against the background of individual susceptibility to the effects of any physical factors during childbirth.
ORIGINAL ARTICLES
Background. One of the most common and severe complications of monochorionic pregnancy is feto-fetal transfusion syndrome (FFTS). The incidence of transfusion syndrome in monochorial diamniotic twins ranges from 10 to 15%.
Objective. To analyze the angioarchitecture of the placenta in FFTS, to determine its features with a favorable and unfavorable outcome after laser coagulation of placental anastomoses (LPCA).
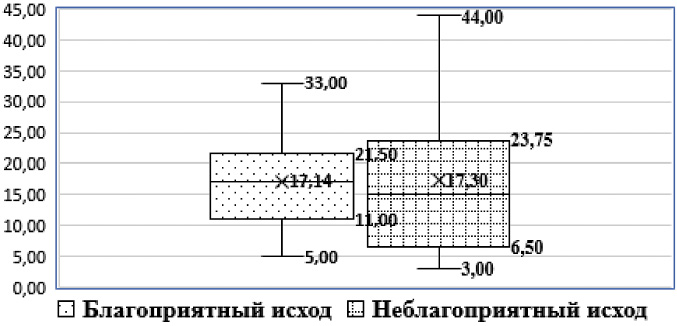
Materials and methods. Continuous prospective, cohort, comparative study 90 pregnant women with monochorionic diamniotic twins were examined: in 60 people (the main group) the pregnancy was complicated by FFTS, in 30 patients (the comparison group) the pregnancy was characterized by a normal course; their newborns and afterbirths. The main group was divided into 2 subgroups depending on the outcome of LCPA in order to correct FFTS: subgroup 1 — favorable outcome (n=50), subgroup 2 — unfavorable outcome (n=10).
Result. The angioarchitecture of the placenta in FFTS with a favorable outcome of LCPA is characterized by the presence of large arteriovenous placental anastomoses in combination with “central-central” and “central-marginal” variants of umbilical cord attachment. A larger number of anastomoses is recorded in monochorionic twins with FFTS and vascular patterns with two or more arteriovenous anastomoses (“Type B” and “Type D”), in our study they were more common with an unfavorable outcome of laser coagulation of placental anastomoses (OR = 5.23 (95%CI 2.13;12.8);p<0.001).
Conclusion. Angioarchitectonics of the placenta in feto-fetal transfusion syndrome with a favorable outcome of laser coagulation of placental anastomoses is characterized by the presence of large arteriovenous placental anastomoses in combination with “central-central” and “central-marginal” variants of umbilical cord confluence.
Introduction. An increase in the number of cesarean sections in the world leads to an increase in cases of formation of scar defects on the uterus, which requires attention and the use of new diagnostic and treatment methods. Studying the healing processes of the myometrium is key to preventing the formation of a uterine scar defect, and improvements in diagnostic methods and surgical techniques can reduce the risk of recurrence of a uterine scar defect.
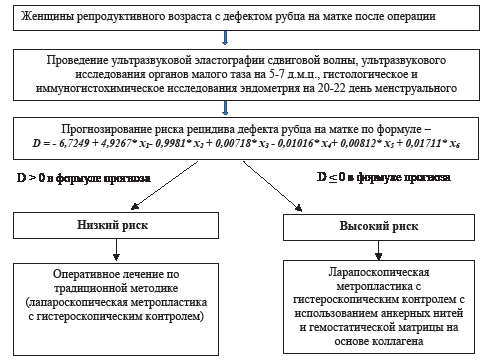
Purpose of the study. To develop an effective algorithm for the management of women with a uterine scar defect at the stage of preparation for pregnancy.
Materials and methods. A prospective randomized cohort study was conducted using a random number generator method with the participation of 100 women with a uterine scar defect after cesarean section. The participants were divided into two groups: in the first group (35 women), surgical treatment was performed using an anchor thread and a collagen-based hemostatic matrix, while in the second group (65 women), surgical treatment was carried out in the traditional way (laparoscopic metroplasty without the use of additional techniques).
Results. A mathematical model has been developed for predicting the risk of recurrence of a uterine scar defect. Using the method of step-by-step discriminant analysis, the most informative predictors of the formation of a recurrent uterine scar defect were identified: shear wave magnitude indicators according to ultrasound elastography, the presence of a cyst in the uterine scar area, the expression of receptors for progesterone and estradiol in the endometrial glands, the expression of CD20 cells and CD138 cells. plasma cells according to an immunohistochemical study of the endometrium.
Conclusion. Understanding the main reasons for the formation of a scar defect and the risk factors for its recurrence will make it possible to more accurately predict the outcomes of laparoscopic metroplasty and choose the most appropriate treatment tactics for each specific patient, which, in turn, can improve the overall treatment results and the quality of life of women
Background. The problem of extremely early premature birth (ERP) is one of the most urgent in obstetrics due to the unfavorable perinatal prognosis and consequences for the mother’s body. At the same time, in the postpartum period, the patient is threatened with infectious and inflammatory complications due to infection prior to childbirth, a decrease in uterine contractility, and prolonged inpatient stay in connection with the care of an extremely premature newborn.
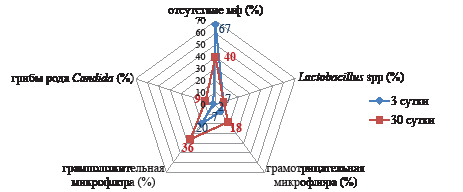
Objective. Assessment of changes in the microbiota of the vagina and cervical canal in women in the dynamics of the first month after extremely early premature birth.
Materials and methods. The main group consisted of women who delivered at 22-27/6 weeks gestation (N=50).The control group consisted of 50 patients who were delivered during full-term pregnancy. The patients underwent bacteriological studies of the contents of the cervical canal and studies of the biocenosis of the vagina by PCR (Femoflor-16). The studies were conducted on the 3rd and 30th days after childbirth.
Results. The microbiota of the lower genital tract of women after extremely early premature birth undergoes the following changes: by the 30th day of the postpartum period, there was a statistically significant increase in the proportion of conditionally pathogenic microflora, mainly represented by gram-positive flora (Staphylococcus spp, Streptococcus spp, Enterococcus faecalis), however, with the development of infectious and inflammatory complications, the proportion of gram-negative microflora increases (Escherichia coli). In the study of vaginal biocenosis, it was found that in the dynamics of the postpartum period in patients after extremely early premature birth, the proportion of aerobic dysbiotic disorders decreases, and the proportion of moderate and pronounced anaerobic dysbiosis increases more than twice.
Conclusion. It is necessary to search for effective methods of preventing postpartum complications of bacterial nature in patients after extremely early premature birth, taking into account the transformation of the microbiota of the lower parts during the first month after childbirth.
Introduction. Chronic endometritis (CE) is reported in 12% of patients with primary infertility. Herpesviruses are considered as one of the causes of CE.
The aim of the study. To evaluate the frequency of herpesviruses DNA detection in endometrium, cervix and vagina in patients with chronic endometritis and endometrial hyperplasia.
Materials and methods. 167 women of reproductive age were included in the study. Samples from the posterolateral wall of the vagina, cervix and endometrium were taken from each patient. The obtained samples were analyzed by real-time PCR for the presence of Herpes simplex viruses type 1 and 2 (HPV 1,2), Epstein-Barr virus (EBV), Cytomegalovirus (CMV) and Human herpesvirus type 6 (HHV6). Endometrial tissue was subjected to morphologic examination.
Results. Depending on the morphology of endometrial biopsy, all patients were divided into three groups: with CE (N=53), with endometrial hyperplasia (EH, N=63), with normal endometrium (N=51). There were no statistically significant differences in the frequency of herpesvirus detection in endometrial, cervical, and vaginal samples. In endometrial samples, EBV was detected in 1 (1.9%) patient with CE (1.9%) and 1 (1.6%) patient with EH, HPV1,2 — in 1 (2%) woman with normal endometrial histology; DNA of other herpesviruses was not detected.
Conclusions. The relationship between herpesvirus type, positive locus and the presence of endometrial pathology has not been established. The frequency of herpesvirus DNA detection in endometrial, cervical, and vaginal samples was not significantly different between the groups of women with CE, EH, and normal endometrial histology. Only 2 (1.7%) of endometrial samples with pathologic morphology were positive for DNA of herpesviruses, in both cases it was EBV.